Diseases Of The Respiratory Units Or Lung Parenchyma
Several widely prevalent respiratory toxicants cause fibrosis or scarring of the lung parenchyma – the internal tissue in the lung – or pleural disease, which is disease of the lung lining. Most cases are due to asbestos exposure, silica and coal dust exposure from working in coal mines, exposure to beryllium (causing chronic beryllium disease), and organic dust (causing hypersensitivity pneumonitis).Asbestos Lung And Pleura Effects
Asbestos is a strong incombustible fiber, which is used for fireproofing and insulation and comprises several forms including chrysotile, amosite, crocidolite, and tremolite. Shipyard workers, electricians, welders, and plumbers all may be potentially exposed. Even moderate, cumulative exposure to asbestos over years can result in various pulmonary manifestations involving either the pleura – the lung lining – and/or the lung parenchyma. Disease may be relatively benign, such as in the case of pleural effusions, a fluid collection between the two layers of lung lining, or pleural plaques – scars of the lung lining studded with calcium deposits. Disease of the lung parenchyma including scarring and pulmonary fibrosis may range from mild to severe. Finally, exposure may cause cancer, primarily lung cancer and mesothelioma (a unique form of cancer of the pleura). Workers with benign disease (e.g., pleural disease) may be asymptomatic, whereas workers with more severe disease (e.g., pulmonary fibrosis) may develop the insidious progression of shortness of breath and nonproductive cough. In the case of the latter, unfortunately, treatment options are limited. Diagnostic evaluation for workers with pulmonary fibrosis may reveal reduced lung volumes – that is, a restrictive ventilatory defect, on lung function tests. Radiographic imaging for workers with pulmonary fibrosis may reveal mild scarring (small, linear, irregular lines) at the lung bases, or bottom of the lungs (Figure 2).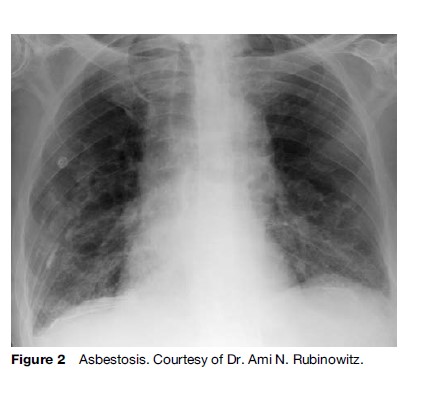
Silicosis And Coal Workers’ Pneumoconiosis
Mineral or organic dust inhalation can result in slowly progressive pulmonary fibrosis. Common causes include coal dust and silica exposure. Less common exposures include talc, kaolin, and mica. Chest radiographs may reveal small rounded opacities that may eventually coalesce into massive fibrosis (Figure 3). Not infrequently, workers may have no respiratory symptoms such as cough or shortness of breath but have significant abnormal findings on chest radiograph.Workers in foundries, tunneling, sandstone grinding, sandblasting, concrete breaking, granite carving, and china manufacturing are exposed to silica. In 1995, the WHO, in conjunction with the International Labour Organization (ILO), launched the International Programme on the Global Elimination of Silicosis. In China, more than 500 000 cases of silicosis and 24 000 deaths were recorded between 1991 and 1995. While acute silicosis has been reported after intense short-term exposure, more commonly chronic exposure by inhalation of quartz or other forms of silica dioxide may lead to a proliferation of small and large rounded opacities and, in some cases, massive pulmonary fibrosis. Lung biopsies combined with energy-dispersive, X-ray analysis may confirm diagnosis but are not generally necessary if given a suggestive history. Two significant complications of silicosis include an increased risk for both lung cancer and active tuberculosis. Pulmonary function tests may reveal reduced lung volumes (restrictive ventilatory defects) associated with a decreased diffusion capacity – that is, a decrease in the ability to absorb and excrete gases. Treatment options for silicosis are limited but may include oral steroids.
Chronic Beryllium Disease
Beryllium is a metallic element found in rocks, coal, soil, and volcanic dust. Exposure occurs in many industries including the aerospace and electronics industries and, to a lesser extent, the dental and laboratory technology and manufacturing ceramics industries. Chronic exposure to beryllium leads to a chronic granulomatous disease indistinguishable from the idiopathic pulmonary disease, sarcoidosis. Workers present with an insidious onset of cough and shortness of breath. In addition to symptoms, diagnosis is made by appropriate radiographs and laboratory demonstration of an immunological response to beryllium from blood or bronchoalveolar lavage (washing from lung). Chest radiographs may reveal small nodular opacities or hilar lymphadenopathy – that is, swelling of the lymph nodes found in the chest. While regulatory agencies in developed countries have reduced exposure levels dramatically, workers at low-exposure levels may still be at risk. Anti-inflammatory therapy such as oral corticosteroids may be effective in symptomatic patients.Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP) is caused by sensitization to organic dusts, particularly fungal or bacterial spores, animal proteins, or chemicals. Farmers, grain operators, wood workers, and bird breeders are at highest risk. HP has acute, subacute, and chronic forms. Acute forms are accompanied by sudden shortness of breath and cough and often improve rapidly after exposure cessation. Chronic disease may occur insidiously or after several acute episodes. Reduced lung volumes (restrictive ventilatory defects) with impaired gas exchange ability (diffusing capacity) are usually present. Chest radiographs may reveal patchy infiltrates or evidence of reticulations and more severe scarring such as honeycombing in more chronic phases. If permanent changes have occurred, exposure cessation may be insufficient. Diagnosis includes taking a suggestive history and a blood test demonstrating immunologic exposure to an appropriate agent. Blood tests, however, are often insufficient as a positive test may simply indicate exposure and a negative test cessation of exposure. Anti-inflammatory medications such as corticosteroids are often particularly useful in the acute setting.Occupational Exposures In Other Industries
Internationally, workers in several other industries not discussed previously are at increased risk for lung disease. The respiratory health of agricultural workers has received increasing attention. Exposure to ammonia, D-glucan, endotoxin, and other microbial products may give rise to several different symptoms including flulike symptoms, shortness of breath, and cough. Asthma and HP are more commonly found. Parenchymal lung disease is also found in workers in other occupations, such as the textile industry, in which exposures to cotton, flax, and hemp dust cause byssinosis. This disease is characterized initially by chest tightness, shortness of breath, and cough. Other reports of those diagnosed with parenchymal lung disease work in the handicraft industries (carpet weaving, brassware, and stone polishing). Finally, tuberculosis (TB) remains epidemic in many countries. Poorly ventilated work spaces may promote TB transmission, and risk is increased by silica exposure.Diagnostic Workup
Diagnostic evaluation includes evaluation of the individual worker, with careful attention to work-related exposures and the presence of disease in coworkers. This section focuses on the key elements of the diagnostic evaluation including history, chest radiograph, and pulmonary function tests. Rarely, more advanced testing such as cardiopulmonary exercise testing or lung biopsies are necessary.Occupational History And Physical
A detailed occupational history is most critical. Information including job title and activities, work exposures, and the extent and duration of exposure is crucial. Former employment history is also key as diseases such as asbestosis and silicosis have a long latency. Any industrial accidents resulting in massive exposure levels should be recorded. The presence of disease among coworkers should be documented. Personal protective equipment (PPE) usage should be determined. Symptomatic improvement while on vacations or during weekends may suggest an occupational etiology, particularly in workers with asthma or HP. Physical examination is often unrevealing, and normal examinations do not exclude the disease. Velcro-popping sounds, occurring as scarred airways open during inspiration, are often heard in workers with chronic parenchymal disease such as asbestosis. High-pitched whistling sounds representing flow through inflamed airways may be heard in asthmatics.Chest Radiograph And Computed Tomography
Chest radiographs are the most important diagnostic test for workers with parenchymal disease. The International Labor Office (ILO classification) first published guidelines for assessing chest radiographs in 1950 and then revised them in 2000. Parenchymal opacities – that is, abnormal shadows in the lung, are classified according to size (large and small), shape (rounded or irregular), extent and profusion (concentration) and are rated on a 12-category scale. Changes in the pleura are also graded. The WHO recommends that workers exposed to silica or coal mine dust undergo chest radiographs at baseline every 2 to 3 years during exposure and every 2 to 5 years after exposure discontinuation. Alternatively, given the long latency of disease, the WHO also recommends increased frequency of chest radiographs in asbestos workers as the time from onset of asbestos exposure increases. Computed tomography (CT) scanning, a more sophisticated diagnostic imaging technique producing detailed cross-sectional images, is more sensitive than chest radiographs. CT scans may help detect early disease and confirm disease in workers with questionable chest radiographs (unfortunately, CT scans require expensive equipment and are often impractical from a logistic and cost perspective).Physiologic Methods
Pulmonary function tests include various breathing tests that measure different aspects of lung function. Organizations such as the American Thoracic Society and the European Respiratory Society have published standards for testing and interpretation. The most routinely and easily administered test is spirometry. During spirometric testing, workers are asked to inhale to full capacity and then exhale forcibly. Decrements in forced vital capacity (FVC, or the amount of total air forcefully exhaled) or in forced expiratory volume in 1 second (FEV1), compared either with the general population or with excessive decrements over time within one individual, are considered significant. In general, a reduction in the ratio of FEV1 to FVC suggests obstructive airways disease, such as asthma or COPD. Individuals without obstruction but reduction in lung volume (FVC), or restrictive lung disease, may have parenchymal lung disease such as asbestosis. Reductions in diffusing capacities (measurement of gas exchange) are also common in parenchymal disease and may occur before reduction in lung volume. Many workplaces require spirometry surveillance. Since significant variation in the population exists, tracking lung function changes in individual workers over time is helpful. The WHO recommends annual spirometry with a workplace intervention if a decline of greater than 15% from the baseline percent of predicted values occurs for certain workforces. Because asthma is episodic, diagnosis can be elusive. Peak expiratory flow rates (PEFR, or measuring how fast a worker can exhale air) measured using a simple portable instrument can be obtained in the workplace and recorded in a diary. PEFR variations between work and home and during vacations or weekends away from work are informative.Exposure
In many countries, workplaces are required to provide employees information regarding the toxicity of workplace chemicals. Workplaces often maintain records of previous and current workplace exposures, which are recorded in material safety data sheets. Historical records contain information regarding changes over time in workplace exposures and records of accidents. Area samples can be obtained by direct air sampling or monitoring devices. Personal samples obtained by attaching devices to workers often provide a better exposure estimation by sampling the worker’s ‘breathing zone.’Prevention, Regulation, And Disability
Prevention
Prevention is the principal strategy used to reduce the burden of occupational lung disease. Prevention may entail toxicant removal, substitution with a less toxic agent, or exposure reduction with or without respirator usage. The health-care worker plays a crucial role in disease prevention simply by recognizing and reporting disease. The patient’s history is the most crucial: the worker’s symptoms should be consistent with the medical, epidemiologic, or toxicologic literature. Exposure should precede disease onset and be of sufficient duration to cause disease. For certain diseases such as RADS, one single massive exposure may be sufficient cause for onset, while for other diseases, such as asbestosis, disease may not present for over 20 years. In certain situations, particularly for asthma or HP, a history of symptom recurrence immediately after exposure and improvement upon exposure cessation is suggestive.Regulation
Several laws and agencies regulate hazardous substance usage in workplaces. Occupational exposure limits (OELs) for short-term and time-weighted average exposures exist for many chemicals. Many countries require surveillance programs and reporting of any occupational diseases. Implementation and enforcement of these limits is challenging. Furthermore, disease, particularly disease related to sensitizers, may occur at chronic, low exposure levels.Disability
A workers’ compensation system exists in many countries and is mandated by law to provide insurance for workers who have been unable to continue working temporarily or permanently due to work-related illness or injury. Impairment is the term for loss of function whereas disability is the term for inability to work because of impairment. Impairment ratings rely on the degree of impairment found on pulmonary function testing. Health-care workers should assess the severity and permanence of the impairment. A long-term assessment is made after a worker has reached maximum medical improvement and is on minimum medication requirements. Specific compensation systems exist for workers in particular fields such as coal mining, cotton workers, and longshoremen. Bibliography:
- Advances in the prevention of occupational respiratory diseases (1998) In: Chiyotana K, Hosoda Y, and Aizawa Y (eds.) Proceedings of the 9th International Conference, October 13–16, 1997. Tokyo: Elsevier.
- Alberts WM and do Pico GA (1996) Reactive airways dysfunction syndrome. Chest 109: 1618–1626.
- American Lung Association of San Diego (1983) Taking the occupational history. Annals of Internal Medicine 99: 641–651.
- American Thoracic Society (2004) Diagnosis and initial management of nonmalignant diseases related to asbestos. American Journal of Respiratory Critical Care Medicine 170: 691–715.
- ATS/ERS Task Force (2005) Standardisation of spirometry. European Respiratory Journal 26: 319–338.
- Banks D and Parker J (eds.) (1998) Occupational Lung Disease: An International Perspective. London: Chapman and Hall Medical.
- Beckett W (2000) Occupational respiratory diseases. New England Journal of Medicine 342: 406–413.
- Chan-Yeung M and Malo J (1995) Occupational asthma. New England Journal of Medicine 333: 107–112.
- Churg A and Green F (eds.) (1998) Pathology of Occupational Lung Disease. Baltimore, MD: Lippincott, Williams and Wilkins.
Our Advantages
- Quality Work
- Unlimited Revisions
- Affordable Pricing
- 24/7 Support
- Fast Delivery
Order Now
