epidemiological Studies Of The Health Effects Of Present-Day Air Pollution
Although subsequent studies linking more routine levels of air pollution and adverse health outcomes are not as obvious, recent epidemiological studies have found statistically significant associations between multiple individual pollutants and a wide range of significant adverse and preventable health effects at present-day pollutant levels in the United States, and sometimes even in areas with pollution levels below current air pollution standards. The acute adverse health effects of air pollution have been shown to include reduced lung function, inflammation in the lung, increased numbers of asthma attacks, excess respiratory and cardiac hospital admissions, and even premature death. The documentation of the adverse effects of chronic exposure to air pollution is not as extensive as for acute effects, but it has been reported to cause the induction of respiratory diseases such as bronchitis and asthma, as well as to cause premature mortality. As a result of a growing body of epidemiological and toxicological studies, the air pollution association with adverse health effects seen in past episodes has been confirmed and better understood to also occur at much lower present-day air pollution levels. Indeed, in the early days of air pollution epidemiology and regulation, it was believed that there was a ‘threshold’ level of pollution below which no effects would be found, but as levels in the ambient air have declined, scientists have yet to find a level of air pollution below which no adverse effects are found. This indicates that increases in air pollution can be expected to proportionally increase the risk of adverse health effects of air pollution among exposed populations. Particulate matter (PM) and ozone (O3) are among the key air pollutants that have been revealed by research to adversely affect human health. As discussed next, the health effects that have been associated with exposure to ambient PM and ozone include a range of morbidity (illness) and mortality (death) effects from both acute and chronic exposure.Health Effects Of Acute PM Air Pollution Exposures
Acute (short-term) increases in air pollution have been found to be associated with increases in the number of daily asthma attacks, hospital admissions, and mortality. In particular, it has been found that PM air pollution is associated with increased risk of respiratory hospital admissions (relative risk (RR) >1.0) in New York City and Buffalo, New York, and Toronto, Ontario, as well as with mortality in cities such as Chicago, Illinois, and Los Angeles, California (see, e.g., Thurston et al., 1992). These results have been confirmed by other researchers considering locales elsewhere in the United States, and in other cities throughout the world (e.g., see Schwartz, 1997; U.S. EPA, 2004). In addition to lung damage, recent epidemiological and toxicological studies of PM air pollution have shown adverse effects on the heart, including an increased risk of heart attacks. For example, when PM stresses the lung (e.g., by inducing edema), it places extra burden on the heart, which can induce fatal complications for persons with cardiac problems. Indeed, Peters et al. (2001) found that elevated concentrations of fine particles in the air could elevate the risk of myocardial infarctions (MIs) within a few hours, and extending 1 day after PM exposure. These researchers found that a 48% increase in the risk of MI was associated with an increase of 25 μg/m3 PM2.5 during a 2-h period before the onset of MI, and a 69% increase in risk to be related to an increase of 20 μg/m3 PM2.5 in the 24-h average 1 day before the MI onset (Peters et al., 2001). Studies from individual cities around the United States and the world have also indicated increased risk of death (RR >1.0) on high PM pollution days in other nations, as well (e.g., see Schwartz, 1997). Epidemiologic research conducted on U.S. residents has also indicated that acute exposure to PM air pollution is associated with increased risk of mortality. A recent nationwide time-series statistical analysis of mortality and PM10 air pollution in 90 cities across the United States indicates that, for each increase of 10 μg/m3 in daily PM10 air pollution concentration, there is an associated increase of approximately 0.3% in the daily risk of death (Health Effects Institute, 2003). Although a 0.3% change in the daily death risk may seem small, it is important to realize that such added risks apply to the entire population, and accumulate day after day, week after week, and month after month, until they account for thousands of needless daily deaths from air pollution in the United States each year. Whereas most past studies investigate the acute effects of the PM mass on human health effects, newer studies are starting to evaluate the mortality impacts of PM by source-specific components (e.g., see Thurston et al., 2005), raising the prospect that we may someday be able to differentiate the relative roles of various pollution sources in the human health effects of PM air pollution.Effects Of Long-Term Exposure To PM
In addition to the acute health effects associated with daily PM pollution, long-term exposure to fine particles is also associated with increased lifetime risk of death, and has been estimated to take years from the life expectancy of people living in the most polluted cities, relative to those living in cleaner cities. The first studies to show this association were cross-sectional studies that compared metropolitan area death rates in high and low-PM cities, after adjusting for potentially confounding factors in the populations, such as age, sex, and race (e.g., Ozkaynak and Thurston, 1987). These results have since been confirmed by cohort studies that followed large groups of individuals in various cities over time that are able to control for potential confounding factors on an individual level. For example, in the Six-Cities Study (which was a key basis for the setting of the original PM2.5 annual standard in 1997), Dockery et al. (1993) analyzed survival probabilities among 8111 adults living in six cities in the central and eastern portions of the United States during the 1970s and 1980s. The cities were Portage, Wisconsin (P); Topeka, Kansas (T); a section of St. Louis, Missouri (L); Steubenville, Ohio (S); Watertown, Massachusetts (M); and Kingston-Harriman, Tennessee (K). Air quality was averaged over the period of study in order to study long-term (chronic) effects. It was found that the long-term risk of death, relative to the cleanest city, increased with fine particle exposure, even after correcting for potentially confounding factors such as age, sex, race, smoking, and so forth. More recently, a study published in the Journal of the American Medical Association shows that long-term exposure to combustion-related fine particulate air pollution is an important environmental risk factor for cardiopulmonary and lung cancer mortality (see Figure 6). Indeed, this study indicates that the increase in risk of lung cancer from long-term exposure to PM2.5 in a city such as New York was of roughly the same size as the increase in lung cancer risk of a non-smoker who breathes passive smoke while living with a smoker, or about a 20% increase in lung cancer risk (see Pope et al., 2002).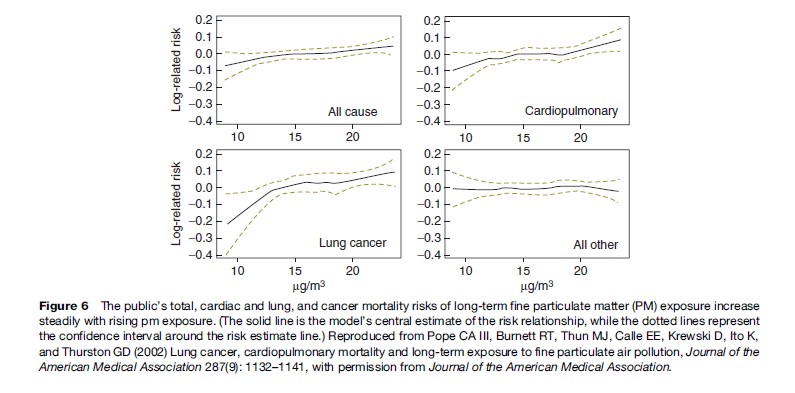
Respiratory Health Effects Of O3
Ozone can irritate the human respiratory system, causing exposed people to cough, feel an irritation in the throat, and/or experience an uncomfortable sensation in the chest area. Ozone has also been shown to reduce the lung’s ability to inhale and exhale, thereby making it more difficult for people to breathe as deeply and vigorously as they normally would (e.g., see Bates, 1995). Research shows that ozone can also acutely aggravate asthma, and new evidence suggests that it may cause more children to get asthma. When ozone levels are high, people with asthma have more attacks that require a doctor’s attention or the use of additional medication. One reason this happens is that ozone makes people more sensitive to allergens, which are the most common triggers for asthma attacks. Ozone can inflame and damage cells that line the air passages of the human lung, and O3 has been compared by some to ‘‘getting a sunburn on your lungs.’’ Ozone may also aggravate chronic lung diseases, such as emphysema and bronchitis, and can reduce the immune system’s ability to fight off bacterial infections in the respiratory system. The nature, sources, and health effects of O3 air pollution have been comprehensively summarized in the U.S. EPA’s ozone criteria document (U.S. EPA, 2006).Health effects of acute O3 exposures
Among the important acute adverse effects associated with ozone exposure to asthmatics is the triggering of asthma attacks. The effects of ozone air pollution on children with asthma have been demonstrated in my own research following a group of children at an asthma summer camp located in Connecticut. This study of a group of about 55 moderate to severely asthmatic children showed that these children experienced statistically significant reductions in lung function, increases in asthma symptoms, and increases in the use of unscheduled asthma medications as ozone pollution levels rose. As shown in Figure 7, the risk of a child having an asthma attack was found to be approximately 40% higher on the highest ozone days than on an average study day (Thurston et al., 1997). Consistent with other research in this area, there is no indication in this plot of a threshold concentration below which children with asthma are safe from the effects of ozone increases.These asthma camp results have more recently been confirmed by a larger study published in the Journal of the American Medical Association. Gent et al. (2003) presented a cohort study of asthmatic children from the New Haven, Connecticut area, including 130 children who used maintenance medications for asthma and 141 children who did not. The more severe asthmatics were identified as those using maintenance medication. For these severe asthmatics, the study found that the level of O3 exposure was significantly associated with worsening of symptoms and an increase in the use of rescue medication. Each 50 parts per billion (ppb) increase in 1-h average O3 was associated with an increased likelihood of wheezing (by 35%) and chest tightness (by 47%). The findings indicate that asthmatic children are particularly vulnerable to ozone, even at pollution levels below the then existing U.S. EPA air quality standards. Acute ozone exposure has also been shown to have adverse effects on athletic performance. Epidemiological evidence compiled more than three decades ago suggested that the percentage of high school track team members failing to improve performance increased with increasing oxidant concentrations the hour before a race (Wayne et al., 1967). Controlled exposure studies confirm this association. For example, Schlegle and Adams (1986) exposed 10 young male adult endurance athletes to 120, 180, and 240 ppb O3 while they exercised for 60 minutes. Although all 10 completed the protocol for filtered (clean) air exposure, 1, 5, and 7 of them could not complete it for the 120, 180, and 240 ppb O3 exposures, respectively, indicating that higher O3 concentrations made exercising more difficult. Epidemiological evidence has accumulated over recent years indicating a role of O3 in daily hospital admissions. Time-series studies conducted in the United States have shown increased risk of hospital admissions (RR >1.0) at higher O3 levels, even after accounting for the effects of PM (Schwartz, 1997). This work has now been expanded to consider 36 cities across the United States, finding that, during the warm season of the year, the 2-day cumulative effect of a 5-ppb increase in O3 was an estimated 0.3% increase in the risk of chronic obstructive pulmonary disease admissions, and a 0.4% increase in the risk of pneumonia admissions (Medina-Ramon et al., 2006). Epidemiological evidence has also accumulated over recent years indicating a role by O3 in daily human mortality. Time-series studies conducted in cities around the world have shown increased mortality (RR >1.0) at higher ozone concentrations, even after accounting for the mortality effects of PM (Thurston and Ito, 2001). More recently, several new multicity analyses have confirmed the ozone–mortality relationship. These include meta-analyses of multiple past ozone studies that show consistent associations between ozone and increases in mortality (Bell et al., 2004; Ito et al., 2005; Levy et al 2005). In one recent new analysis of some 95 U.S. cities over two decades published in the Journal of the American Medical Association, Bell et al. (2004) showed that, even after controlling for PM and weather, an increase of 10 ppb in daily ozone pollution was associated with approximately a 0.5% increase in daily risk of death. As discussed earlier, this percentage increase in daily admissions, though small, affects a huge portion of the population and accumulates day after day to the point that it accounts for thousands of deaths each year in the United States.
Health Effects Of Long-Term Ozone Exposure
Ozone may also cause permanent lung damage. Repeated short-term ozone damage to children’s developing lungs may lead to reduced lung function in adulthood (e.g., see Daily 1-h maximum ozone concentration (ppb) Kunzli et al, 1997). In adults, ozone exposure may accelerate the natural decline in lung function that occurs as part of the normal aging process (e.g., see Detels, et al., 1987). One important new investigation, the California Children’s Health Study, suggests that long-term ozone exposure can increase the chances that children will develop asthma disease. The O3–morbidity associations indicated by the epidemiological studies just presented are also supported by a large body of data from controlled human exposure studies that have demonstrated pathways by which ozone can damage the human body when breathed. Clinical studies have demonstrated decreases in lung function, increased frequencies of respiratory symptoms, heightened airway hyper-responsiveness, and cellular and biochemical evidence of lung inflammation in healthy exercising adults. For example, controlled exposure studies have found that prolonged controlled exposures of exercising men to levels of ozone common in present-day United States (only 80 ppb) resulted in significant decrements in lung function, induction of respiratory symptoms, increases in nonspecific airway reactivity, and cellular and biochemical changes in the lung (e.g., see Devlin et al., 1991).
Our Advantages
- Quality Work
- Unlimited Revisions
- Affordable Pricing
- 24/7 Support
- Fast Delivery
Order Now